
Medical coding is the most underappreciated aspect of medical billing, even though it is essential to revenue cycle management. According to the study report, the revenue cycle’s documentation and medical coding systems are expected to be the worst as time goes by. Medical claims will be processed promptly, and reimbursements will be received swiftly if the medical coding is accurate. The scarcity of medical coding experts is one of the industry’s biggest problems.
The claim cycle’s essential element of medical coding is required for claim reimbursement. Incorrect coding can negatively affect your practice, including missing income opportunities, potential overpayments, and accusations of reimbursement policy abuse. As the need for follow-up on claim denials grows, inaccurate coding may also cause personnel issues.
Your organization’s bottom line will undoubtedly be impacted by inefficient coding techniques, backlogs, and a tight budget, primarily if you also deal with a small staff and inefficient processes.
It is essential to take the time to examine your coding department because the efficiency of the revenue cycle is significantly impacted by medical coding. You can use it to uncover money lost because discharges weren’t completely billed or to lower denials because of coding issues.
Your sales cycle is a continuous process. Many of the coding-related problems you find during the initial round of analysis and corrections can be solved at a high level. To ensure that the issues won’t reoccur, you must continuously examine your coding quality and make structural improvements.
Improving Medical Coding
Leveraging And Use Of Modern Technology
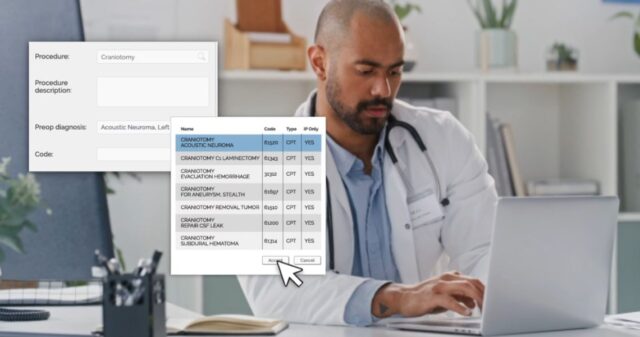
Medical coding underwent a revolution due to electronic health records, which transformed the once paper-based procedure. Other technologies have arisen to enhance the caliber and accuracy of medical coding, even if the EHR system is still essential to the process.
For instance, computer-assisted coding (CAC) solutions are medical office software programs that can examine medical records to determine the proper medical codes for the clinical material contained in the records. The solutions improve efficiency and accuracy while speeding up the medical coding process.
Doctors should continue to turn to their EHR systems for support with accurate medical coding. The technologies used to keep electronic health records have changed just as medical coding did with the introduction of those records.
In a value-based environment, providers should ensure EHR systems can capture all the information coders require for an accurate and entire claim.
Coding Quality Audits As A Process
Technology has simplified medical coding, but coding quality audits are still a crucial part of a comprehensive plan for improving medical coding.
These “soft” denials that demand further information for reimbursement can be avoided by making sure medical coding procedures adhere to the payer code. Internal audits of these procedures can spot instances or categories of situations where income is lost due to poor practices, inefficient workflow, or even a lack of training.
Identified variations may or may not point to possible abusive or fraudulent billing and coding methods. Deviations must first be further analyzed to ascertain whether there is a compliance issue.

Opening Communication Lines
Providers should notify coders as quickly as possible of audit results and any changes in coding compliance. Coders can change procedures right away to enhance coding quality by communicating places that can be improved. Additionally, communication ensures that coders are aware of updates to coding compliance, particularly when the unexpected occurs.
To achieve significant change for the enhancement of coding quality, audit results should be communicated to doctors and anyone involved in the revenue cycle. Engaging stakeholders at every stage of a case’s journey before coding will help to create a smooth revenue cycle because coding affects every phase of the revenue cycle after it.
Since clinicians are responsible for recording clinical encounters that will be converted into reimbursement claims, sharing audit findings and coding compliance modifications with them can be extremely helpful.
The healthcare sector should also be ready for such occurrences. As providers transition to value-based compensation, ensuring medical coding quality will be essential for receiving payment for services and accurately documenting the standard of care.
Challenge Your Sources
On the other hand, many poor or inaccurate resources are available. It doesn’t make something accurate just because someone wrote it on the internet or elsewhere. Coding is challenging, and it’s important to remember that reducing medical care to a string of five-digit numbers isn’t an exact science. There will be divergent viewpoints. The resources that have been confirmed and verified will typically be a little more cautious. Similar to this, other too-aggressive resources are available that might not have a solid base. When in doubt, pay attention to where you are reading what you are reading, and if what you read agrees with you, don’t stop reading it.
Additionally, be cautious about where you purchase your coding books. Remember that the funds backing your Ingenix book are the same ones that support your pals’ high salaries at the UHC corporate headquarters. Call me cynical, but it seems like there might be a small amount of inherent ethical conflict involved in running a business that processes/pays codes while also assisting in paying physicians. It doesn’t seem right to me, and any book on coding will likely include extrapolation or interpretation outside of the AMA guidebooks.

Invest In Your Resources
Medical coding is a laborious process that calls for much training and expertise. Implementing standard coding is still another demanding endeavor that calls for talent on top of that. A committed programmer must be involved in evaluating the current coding practices.
As a result, practices, and revenue cycle managers must select medical coders who can manage training and immediately implement changes. Medical coders must follow the organization’s coding guidelines and make any necessary transitions.
Use materials other than your AMA coding book. It sounds obvious and should probably go without saying, but it is essential to do so. NCCI modifications are frequently disregarded in the coding process, but they are an excellent tool to determine whether your coding choice is accepted as payment on the same service date. Additionally, the CMS Physician Fee Schedule Search Tool is a fantastic tool for locating global periods, assistant/co-surgeons, and other relevant information.
The AAPC coding forums are great for finding peers dealing with related problems. Don’t forget to look at the societies related to your field of study; the AAD and the ASPS provide excellent resources. Many other cost-free resources are available online, including global period lookup calculators and CPT search engines.
Assemble A Coding Team
Most healthcare professionals favor doing all of their medical coding for small practices. Medical coding, however, entails more than merely selecting the appropriate procedure codes and invoicing them. Medical coding requires payer-specific paperwork, precise procedural code selection, proper modifier selection based on clinical circumstances, appeals of denials with the necessary supporting data, and coding audits to ensure compliance with payer coding standards.
Because they are so busy providing inpatient care, physicians don’t have enough time to stay updated on coding updates and payer-specific rules. Therefore, allowing coding specialists to handle medical coding on your behalf is preferable.

Regular Updates To The Rules And Coding
Verify that your EHR complies with the newest code updates. If not, take steps to modify the system to meet the demands. Update coding standards and guidelines to preserve transparency and enhance EHR/PMS compliance with the most recent regulations.
These are essential components to update to prevent your practice from applying coding requirements erroneously, which would increase the number of denials.
Speed Up The Documentation Process
The effectiveness of the medical coding process is significantly influenced by how accurate the paperwork is. It is also the simplest way to increase reimbursements and the effectiveness of the coding process. If your practice is experiencing problems achieving the necessary accuracy in its documentation, speak with a Clinical Documentation Improvement (CDI) specialist.
Follow EMR workflows
It takes time and requires a lot of research, amending, and resubmitting to handle claim denials. Your data on claim denials can be analyzed to help you find coding issues that come up regularly.
If not twice a month, at least once a month, review coding denials with your coding team to identify the primary factor behind the top 5 to 10 code-related denials. It typically results from insufficient clinical paperwork in the hospital or a lack of understanding of the correct codes for surgery. A brainstorming session can instruct programmers on good coding techniques and assist you in finding solutions to many of the current coding problems.
You may speed up cash flow while avoiding repeating the same mistakes by developing system-driven validations.
Limit Non-Coding Tasks For Your Developers
Do any of your coders handle front-end business tasks like booking appointments or helping patients check in? Limit the non-coding work your coders do so that there can be a stronger emphasis on what they do best. It is vital to remember that programmers are occasionally best suited to additional jobs. There are several advantages to carefully reviewing work assignments to evaluate if non-coding tasks are better placed with non-coding workers.
For instance, highly compassionate coders with a talent for translating complex medical terminology into simple terms would be the ideal choice to respond to patients’ inquiries about coding.
You must thoroughly examine your coding team’s organization, procedures, and systems if you want to address coding quality issues. And to succeed with the coding strategy, practices must adhere to the proper guidelines.

Conclusion
To earn money, it’s critical to ensure accurate medical coding. So the only things left to do are to verify credentials, check for quality, and inform.
A team of professional coders can resolve many problems causing a large number of coding denials. Correct reimbursements depend on correct medical coding. Claims denials, unnecessary compliance problems, and financial ruin can all be brought on by medical coding errors.
Your coding team’s structure, procedures, and systems must be thoroughly reviewed to address code quality issues. A high-quality coding team can develop a sustainable approach to providing high-quality coding services, and code audits can help you uncover the problems.









